Diabetes can affect many parts of the body, including the eyes. One of the most serious vision-related complications linked to long-term diabetes is diabetic retinopathy, a condition caused by damage to the blood vessels of the retina. Because early stages often present with few or no symptoms, awareness of warning signs is essential for preventing permanent vision loss.
Understanding how symptoms of diabetic retinopathy disease develop and progress empowers individuals with diabetes to seek timely eye care and protect their sight.
What Happens to the Eyes Over Time
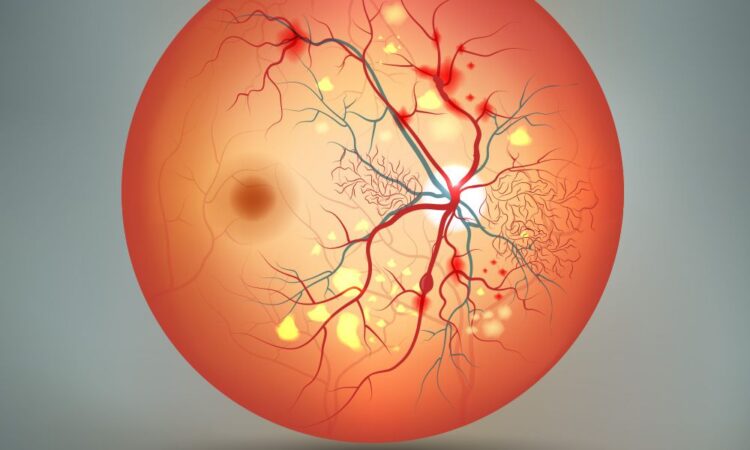
Chronically elevated blood sugar levels can weaken and damage the tiny blood vessels that supply the retina.
As these vessels become compromised, they may leak fluid or bleed, interfering with normal vision. In more advanced stages, abnormal new blood vessels may grow, further increasing the risk of vision problems.
These changes usually occur gradually, which is why regular eye examinations are crucial even when vision seems normal.
Early Symptoms That Are Easy to Miss
In its initial stages, diabetic retinal disease may not cause noticeable discomfort.
Many people maintain clear vision while retinal damage slowly progresses. This lack of early symptoms often leads to delayed diagnosis, especially in individuals who feel their diabetes is well controlled.
Occasional mild blurring or difficulty focusing may occur, but these changes are often mistaken for normal eye strain or aging.
Common Visual Changes to Watch For
As retinal damage advances, visual disturbances become more apparent.
Blurred or fluctuating vision is one of the most frequently reported symptoms. Patients may notice difficulty reading, recognizing faces, or seeing details clearly.
Colors may appear faded or washed out, making everyday tasks such as driving or reading labels more challenging. These changes should never be ignored, especially in individuals with a history of diabetes.
Floaters and Dark Spots in Vision
Another warning sign involves the sudden appearance of floaters.
Floaters look like small dark spots, strings, or cobweb-like shapes that drift across the visual field. They are caused by tiny amounts of blood or debris leaking into the vitreous humor of the eye.
While occasional floaters can be harmless, a sudden increase may indicate retinal bleeding and requires prompt evaluation.
Vision Loss and Blind Spots
As damage becomes more severe, areas of vision loss may develop.
Blind spots or dark patches can appear in central or peripheral vision, making it difficult to see objects clearly or navigate safely. These areas may expand over time if left untreated.
In advanced cases, significant vision loss can occur, potentially leading to legal blindness if intervention is delayed.
Symptoms of Advanced Disease
In later stages, symptoms tend to worsen rapidly.
Sudden vision loss may occur due to extensive bleeding inside the eye or retinal detachment. Patients may experience severe blurring or the sensation of a dark curtain covering part of their vision.
These symptoms represent medical emergencies and require immediate attention to prevent permanent damage.
Risk Factors That Increase Symptom Severity
Certain factors can accelerate disease progression and intensify symptoms.
Poor blood sugar control, high blood pressure, and high cholesterol levels place additional stress on retinal blood vessels. The longer a person has diabetes, the higher the risk of developing serious eye complications.
Pregnancy and smoking can also worsen retinal changes, making regular monitoring even more important.
Importance of Regular Eye Examinations
Because symptoms may not appear until significant damage has occurred, routine eye exams are critical.
Comprehensive dilated eye examinations allow eye care professionals to detect early retinal changes before vision is affected. Early detection enables timely treatment and better long-term outcomes.
Even individuals with stable vision should undergo regular screening as recommended by their healthcare provider.
When to Seek Immediate Medical Attention
Certain symptoms should prompt urgent evaluation.
Sudden vision changes, a rapid increase in floaters, flashes of light, or partial vision loss are all warning signs that require immediate care. Prompt treatment can prevent further damage and preserve remaining vision.
Ignoring these symptoms can result in irreversible complications.
Conclusion
Recognizing symptoms and warning signs is a key step in protecting eye health for individuals living with diabetes. While early stages may be silent, progressive changes can significantly affect vision if left untreated.
Through awareness, regular eye examinations, and timely medical care, diabetic retinopathy can be detected early and managed effectively, helping patients maintain their quality of life and visual independence.